Stephen’s strength under stress led him to receive the Ed Block Courage Award. Tiffany earned her doctorate and came through post-traumatic stress disorder to create Skyler’s Gift Foundation along with her husband. The nonprofit aids unprepared families in paying for the funerals of premature infants who don’t survive. The organization also provides funding for those families’ grief counseling.
In recalling the loss of young Stephen, the couple reflected upon the worry and grief they felt – but also the dedication of their sons’ health care providers. People who work in the NICU “are heroes,” Tiffany emphasized.
NICU Safety
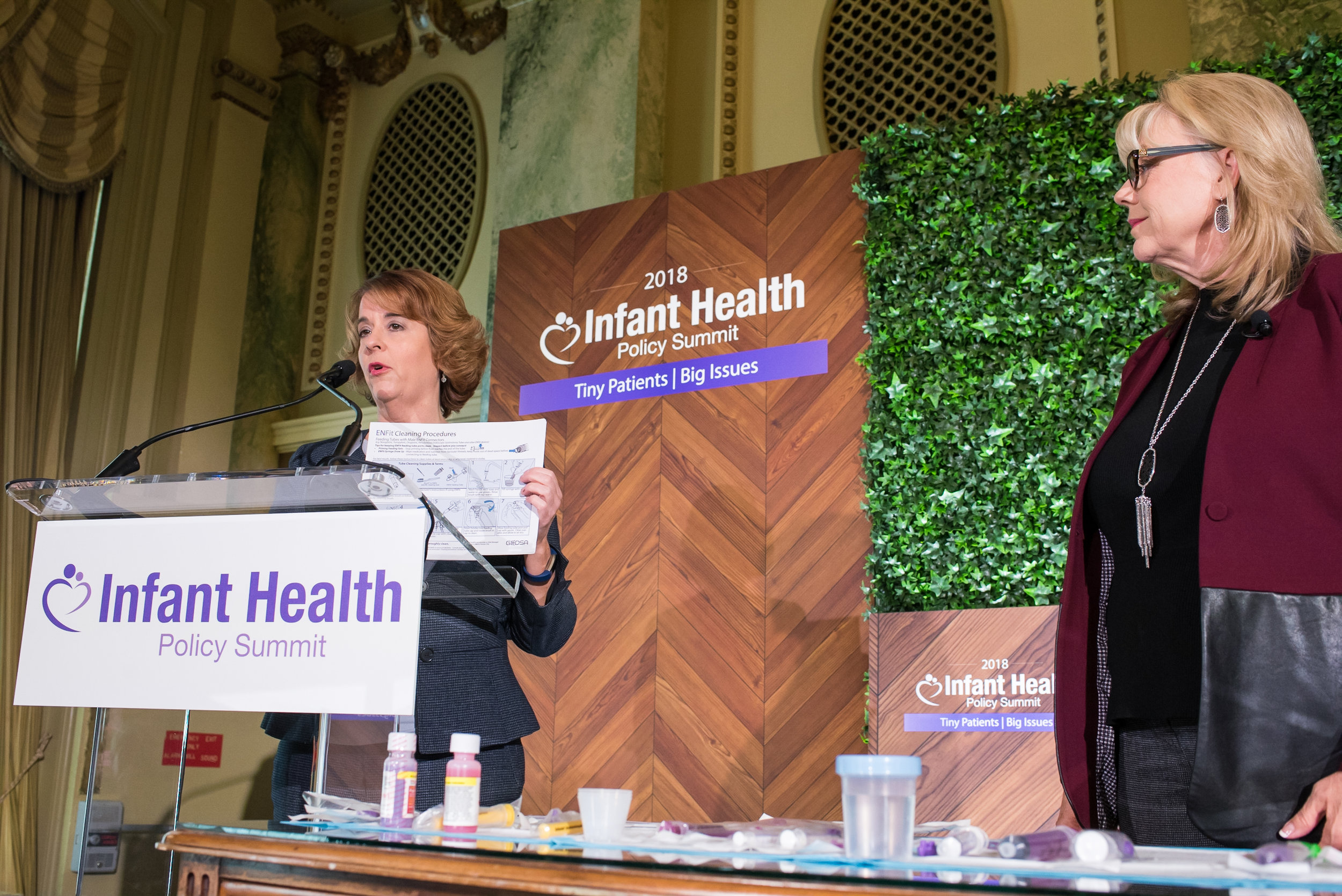
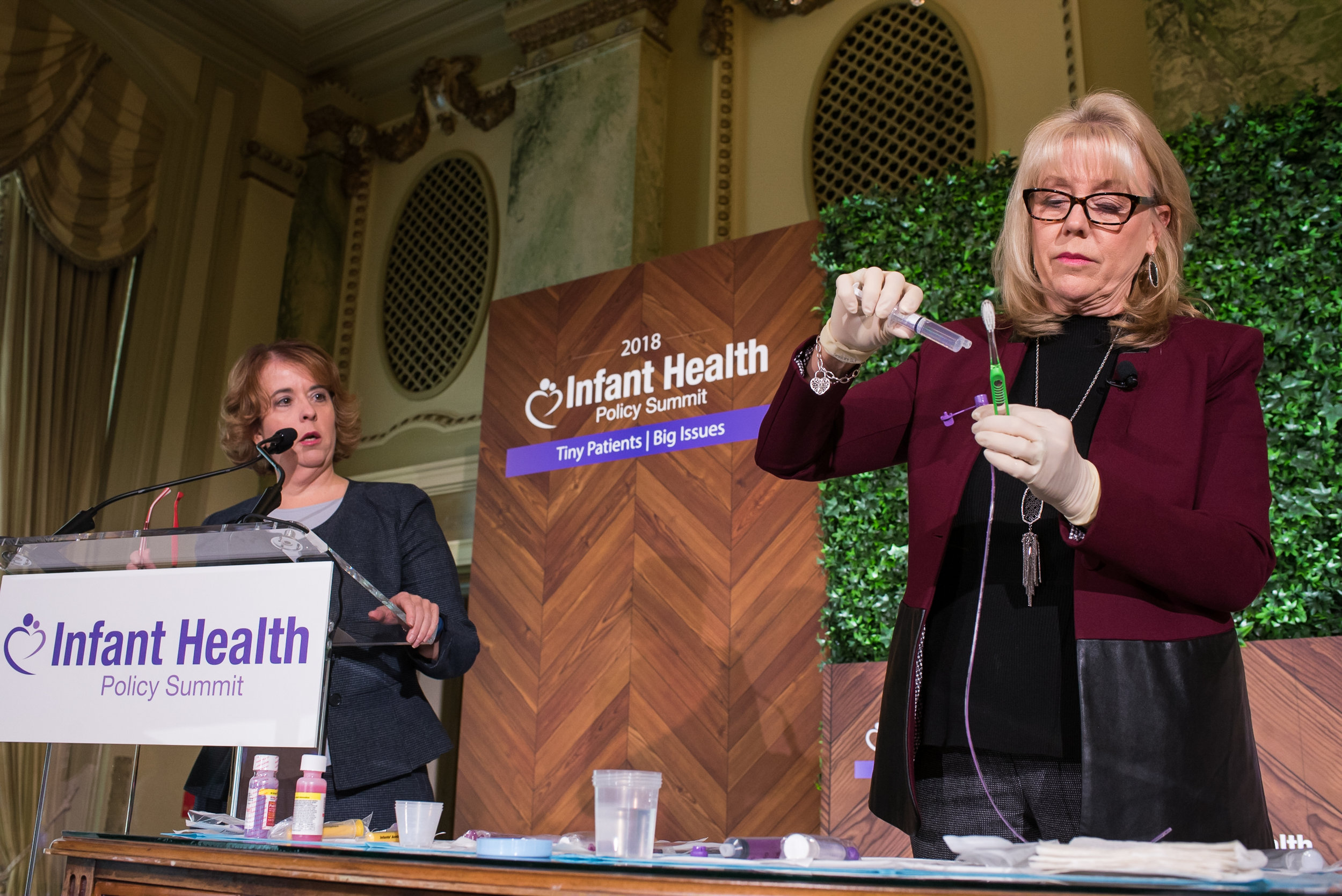
Those heroes face challenges of their own. Just consider the issue of hospital tubing. Addressing the summit audience, Rebekah Thacker, MSN, of the University of Arkansas Medical Center described concerns about the use of tubing connectors known as ENFit in NICUs. As described in a 2017 video from the National Coalition for Infant Health, liquid can “hide” in the reservoir at the tip of the connector – potentially dosing tiny infants with more medication than intended.
Thacker described her efforts to push back against industry’s drive for ENFit adoption. “Nobody knows the neonatal population like a neonatal nurse,” Thacker insisted.
“Still a Preemie”
And that population is broader than one might expect. The National Coalition for Infant Health released at the summit a new video emphasizing the full spectrum of prematurity. “Still a Preemie,” explains that preemies don’t always conform to stereotype. Late-preterm infants born from 34 through 36 weeks’ gestation, or those who are born premature but at a “normal” birthweight, can still struggle with feeding issues, jaundice, respiratory conditions and development delays. And their parents can feel the effects too.
Just ask Kelli Kelly of the parents support organization Hand to Hold. When Kelly’s daughter Lauren was born at 34 weeks, she “looked good, looked healthy” Kelly recalled in an address to summit attendees. But the appearance was deceiving. Lauren required NICU care, so Kelly left the hospital “with empty arms.” She recalled waking during the nights to pump breastmilk for her daughter, whose developmental challenges made it impossible to breastfeed. Kelly suffered emotionally. “It’s hard to bond with a baby that’s in a glass box,” she recalled.